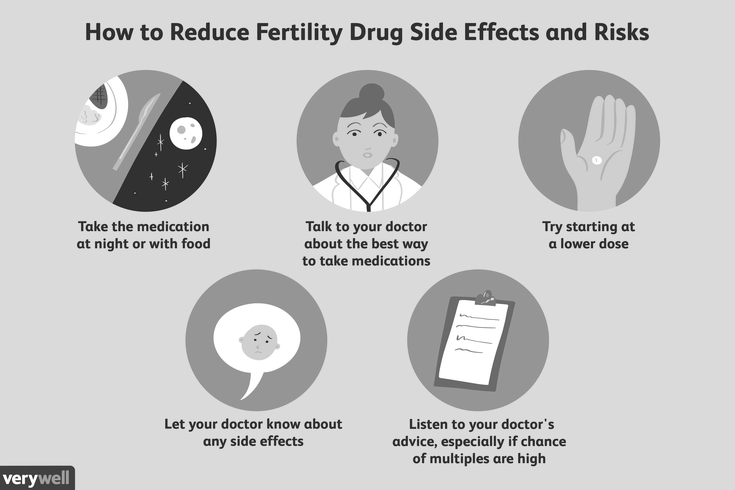
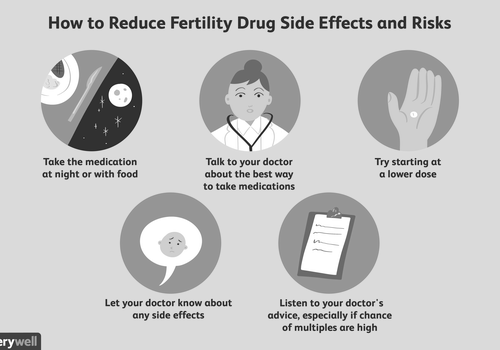
To minimise the risk of side effects, you should carefully read the medication label and talk to other people who have the same condition as you. You can also find reliable resources online. Also, ask about alternatives to the medication. Some new medications have side effects that you may not be aware of. This is why it may be a good idea to switch to an older, proven drug.
Common side effects of prescription drugs
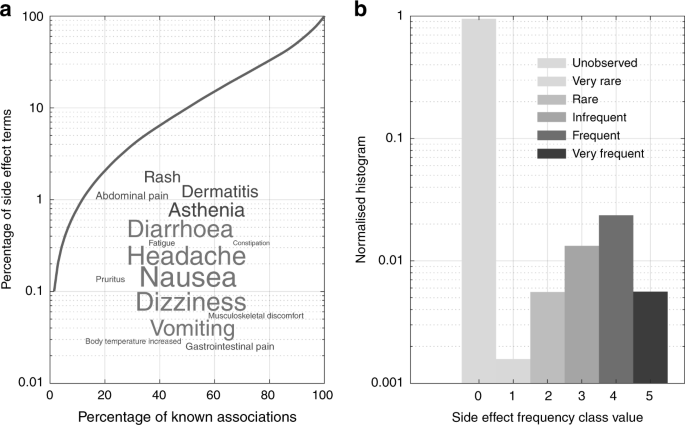
Common side effects of prescription drugs are unpleasant or harmful reactions caused by a medication. While most of them are minor and are only a nuisance, more severe side effects may require medical attention. In some cases, these side effects may lead to death, disability or birth defects. For these reasons, it is important to follow your doctor’s prescription for the medication.
Symptoms of common side effects include muscle aches, headaches, drowsiness, nausea, and upset stomach. Some drugs can even cause your urine to turn blue. If you experience any of these effects, contact your doctor immediately. In addition, you should discuss with your healthcare provider any allergies you may have.
Prescription drugs are commonly used to treat and prevent disease. They are highly effective in treating most illnesses and are even able to prevent or cure some of them. The pharmaceutical industry is a billion-dollar business, and more than four-fifths of Americans take at least one prescription drug. While medication is highly beneficial, it comes with side effects.
A side effect is an unexpected reaction to a drug. While most side effects are mild and go away on their own after a person stops taking it, others can be severe and last for months. Some medications can cause allergic reactions that are life-threatening. These reactions can range from a runny nose to a heart attack. There are ways to combat side effects and avoid them altogether.
Prescription drugs may also cause erratic behavior and mental cloudiness. For instance, people who abuse prescription drugs may become easily confused or appear to be unable to sit still for any length of time. They may also lose interest in personal hygiene or clothing style. This can lead to isolation and vulnerability.
If you notice any of these side effects, talk to your health care provider immediately. They can help you manage these side effects by altering your dosage or prescribing an alternative medication. They may be able to help you reduce these side effects or help you stop taking the drug altogether. The best way to minimize these side effects is to talk with your healthcare provider and learn more about them.
Prescription drugs are dangerous and have many side effects. While a few are mild, others can become habit-forming and cause addiction. This is why it is crucial to be aware of the side effects before starting a new medication. These side effects can occur at any time, including when the drug is first taken, after a change in dosage, or if the medicine is stopped abruptly. Also, a medication can interact with other medications, causing a dangerous reaction.
Drug-gene testing reduces drug side effects
As the number of hospitalizations caused by severe drug reactions rises, researchers are looking at ways to reduce them. One such way is genetic testing. It can help doctors predict which patients are most susceptible to certain drug side effects and help them tailor their treatment. Moreover, it may improve health care efficiency and cost. It may also improve patient safety.
Pharmacogenomics, also known as genetic testing, involves studying the role of genes in the metabolism of medicines. Since DNA plays a role in drug response, dosage, and metabolism, it is essential to understand how different individuals respond to specific medications. A DNA-based drug-gene test called RxMatch can help doctors find out if patients are at risk of adverse effects. The test is available from your primary care provider and includes details about the medications you take, including antidepressants, antidiabetics, and other medications.
Drug-gene testing has been proven to reduce drug side effects. It can also help doctors determine which dosages are the most appropriate for individuals. Drug-gene tests are also used to determine the efficacy of medicines. The results of the tests can be used to tailor a person’s treatment based on his or her unique genetic makeup.

Although genetic testing is expensive and is not suitable for all drugs, it helps doctors optimize drug therapy. Genes control the production of proteins, and most drugs target these proteins. However, genes are polymorphic, and some variations can alter their function. This means that some drugs will cause more side effects, while others may cause no reaction at all. Genetic testing is not necessary for most drugs, but for certain drugs, the tests can prevent life-threatening side effects.
Currently, most drug-gene tests are conducted to minimize or prevent severe adverse effects. However, before the advent of modern genetic testing, such tests were not affordable, time-consuming, or specific enough. But thanks to improvements in genetic technology, it has become possible to test all genes with just a small amount of DNA. Furthermore, the technology has advanced enough to enable rapid results.
Contact your healthcare provider if you experience a side effect
If you are taking a medicine for a medical condition, it is important to be aware of any possible side effects. These effects can range from minor irritation to serious adverse events. Some are expected, and others may occur in very rare cases. You should contact your healthcare provider if you notice any of these side effects.
While these effects are generally harmless, some can be life-threatening. These include liver damage and severe bleeding. They can also prevent you from driving or other activities. If you experience any side effects, write them down and inform your healthcare provider as soon as possible. If you’re concerned about any particular side effect, call your healthcare provider and request a change in medicine.
Some side effects may occur after several weeks of taking a medicine. It may be best to contact your healthcare provider if you experience these symptoms, especially if they happen too often or are severe. The healthcare provider can advise you on other medicines that can help you manage the side effect.
It is important to tell your healthcare provider about all medicines you’re taking. Include over-the-counter drugs, herbal remedies, and supplements. You can discuss any interactions or allergies you may have with other medicines. Your health care provider may be able to prescribe you a better medicine or even prescribe you a different medication.
In addition to side effects caused by medicines, other herbal supplements may also interact with them. For instance, ginseng, garlic, and ginkgo biloba can interact with some medicines. These substances can change the way your body metabolizes the drug.
Before you begin a new medicine, make sure you know the dosage for the medicine and which foods or supplements you should avoid during its use. It is also important to discuss any side effects with your health care provider, because some may be signs of a dangerous interaction with another medicine.
Side effects of medicines should be reported to your healthcare provider or pharmacist. Your pharmacist can also advise you on the best ways to manage the side effects. For prescription medicines, you should read the patient information on the drug’s label. This information may also help you decide whether to take the medicine with or without food or drink.
If you have a chronic illness, keep a record of all the medicines you’re taking. This list should include the name of the medicine, the dose, and how long you’ve been taking it. It should also include the name of the doctor who prescribed the medicine and the reason. When you are concerned about a side effect of a medicine, you can also report it to the Food and Drug Administration’s MedWatch program. The reporting process is free, confidential, and secure. If you have experienced an adverse reaction to a medicine, your information may help prevent other people from experiencing the same problem.
A side effect of medicine can be life-threatening and can even be fatal. If you notice an adverse effect, it is best to contact your healthcare provider immediately.
Ciprofloxacin is a prescription drug that treats bacterial infections. It is generally safe for humans, but there are some possible side effects. People should always take ciprofloxacin in the prescribed form and dosage. Inadequate dosage can lead to serious complications, including acute renal failure and an intestinal infection caused by Clostridium difficile. Although there are no documented reports of harm to a developing fetus, there is still some uncertainty regarding its use in pregnancy.
ANCA-negative cutaneous and renal vasculitis
Ciprofloxins are antibiotics that can cause adverse reactions in patients. One such adverse effect is ANCA-negative cutaneous and renal vasculitis. This rare condition is caused by the formation of autoantibodies to the proteinase 3 enzyme. This enzyme causes damage to blood vessels in the skin.
The disease has many causes and may be autoimmune or inflammatory. Symptomatic patients may experience skin purpura, arthritis, and nephritis. It may also be associated with lung adenocarcinoma and mesothelioma. However, it is not known whether ciprofloxins cause this condition.
The symptoms of ciprofloxacin-induced cutaneous vasculitis can be fatal. Symptoms typically appear three to five weeks after exposure to ciprofloxacin. The disease is difficult to diagnose and has a high mortality rate. However, the disease can be treated effectively by stopping the antibiotic.
In addition to cutaneous and renal vasculitis, ciprofloxins can also cause leukocytoclastic vasculitis. This is an inflammatory disease of the small blood vessels that is mediated by immune complexes. The symptoms include palpable purpura and inflammatory infiltration.
An 63-year-old man with type 2 diabetes presented with an erythematous rash. This began three days after he began taking levofloxacin 500 mg twice daily. The patient was also not experiencing hematuria or abdominal pain. He had a history of penicillin allergy. The patient was otherwise healthy, with a normal blood pressure and respiratory rate.
Changes in sensation and nerve damage
The long-term use of ciprofloxins is associated with a risk of nerve damage and changes in sensation. These side effects may persist for months even after stopping the medication. They may lead to pain, numbness, or tingling in the arms and legs.
Ciprofloxacin may cause serious side effects, particularly for people with neurological disorders. It may cause seizures or epilepsy, and should be avoided in individuals with such conditions. Ciprofloxacin may increase sensitivity to sunlight and cause sunburn. For this reason, it is essential to wear protective clothing or use sunscreen when outdoors.
Another major adverse reaction to ciprofloxins is tendinitis and tendon rupture. Although it is rare, tendinitis can be severe and potentially disabling. Tendinitis and tendon rupture have been associated with FQ antibiotic use for over 25 years, and the FDA has updated its labeling to warn of this risk. Since the drug was first introduced in the 1970s, several reports have linked the drug to early-onset and permanent nerve damage.
Cipro is an oral medication for the treatment of bacterial infections. It is available as an oral tablet or as an oral solution. Typically, a treatment course lasts seven days. It is important to complete the entire course of the antibiotic. Early discontinuation may lead to the infection reoccurring.
Formation of crystals in urine
Ciprofloxacin may cause the formation of crystals in the urine in both healthy and diseased individuals. However, crystalluria is rare in humans and is more common in laboratory animals. In addition, it can increase potassium levels in the blood. For these reasons, the drug should be administered with caution.
The study included five female patients who developed acute ciprofloxacin intoxication. All patients were age 22 or older, and four had histories of psychiatric disorders. One had a history of diabetes, and another had a recurrent urinary tract infection. The patients were recruited by telephone or in-person through community care centers. Each participant was randomly assigned to receive either oral or intravenous ciprofloxacin. Randomization was carried out using sealed envelopes, and the study protocol was approved by the local ethics committee.
Ciprofloxacin tablets should be taken with a meal. It is important to avoid taking these tablets with dairy products or calcium-fortified juices. However, if this is not possible, the patient should continue to receive the prescribed dose on a regular basis.
Another serious side effect of Ciprofloxacin tablets is hepatotoxicity. In some cases, this can result in a serious complication called acute hepatitis. In rare cases, this condition may even be fatal. Therefore, patients should immediately inform their doctors if they experience any of these symptoms. Some of the common symptoms of liver damage include nausea, loss of appetite, or arthralgia. Additionally, patients should be concerned if they develop symptoms of itching or yellowing of the skin.
Increased risk of Achilles tendinitis and rupture
In this study, the researchers found that the use of ciprofloxins increased the risk of Achilles tendinitis and Achilles tendon rupture. The study was conducted on patients with a history of Achilles tendon pain and rupture. The study population was composed of patients aged 18 to 95 years, with a median age of 48 years. The study excluded patients with prior history of cancer, AIDS, or alcoholism. In addition, the researchers reviewed the medical histories of these subjects without knowing the type of drug they had been taking.
Previous observational studies have found an increased risk of tendon rupture associated with fluoroquinolones. However, these studies have not been large enough to draw definitive conclusions. Some of the studies used case-control designs and reported very low rates of rupture. In contrast, a case-control study in Italy showed a 30% risk of Achilles tendon rupture among participants taking fluoroquinolones.
The study also included a 63-year-old man who had previously taken ciprofloxacin for a urinary tract infection. After taking antibiotics for three months, he developed increasing pain in his Achilles tendon. He was eventually diagnosed with a severe form of Achilles tendinitis, and required ongoing treatment. Although this case is unusual, it illustrates the importance of considering the risk-benefit ratio when taking antibiotics.
The study also examined a case-crossover study where a patient serves as a control. This study used a composite of antibiotics as a negative control, weighted towards milder cases of urinary tract infections. Another study used a cohort design with an active comparator of amoxicillin exposure, and showed an increased risk of tendon rupture among patients treated with fluoroquinolones. The study has potential for residual confounding that may make it difficult to determine the validity of the relative risk.
Increased risk of propriospinal myoclonus
Increased risk of propriospinal myaclonus associated with ciprofloxins has been reported. This movement disorder occurs in the muscle corresponding to the myelomere and may spread to the other myotomes. It is rare and is not thought to be associated with infection by SARS-CoV-2.
Propriospinal myoclonus is a sleep-onset disorder characterized by sudden axial jerks. These episodes often occur during the transitional period between wakefulness and sleep. Polysomnography is necessary to diagnose this condition.
Historically, propriospinal myoclonus has been treated with medical therapies and largely responded well. However, there are currently no specific guidelines for its management. In one recent case, a patient with distractable myoclonus presented with concomitant myelopathy and unresponsiveness to medical therapy. On EMG and MRI, she was diagnosed with PSM.
Increased risk of peripheral neuropathy
Patients who have taken fluoroquinolone antibiotics for longer than six weeks have a greater risk of developing peripheral neuropathy. This side effect may occur in up to four percent of patients taking these medications. Fluoroquinolone antibiotics are used to treat bacterial infections, including pneumonia, urinary tract infections, staph infections, and E. coli. However, the risks of peripheral neuropathy are not well understood. In the meantime, patients who take these medicines should consult their physician for further medical advice.
Fluoroquinolones are widely prescribed antibiotics, and are effective in treating a wide range of bacterial infections. These drugs are commonly prescribed for respiratory, urinary tract, and gastrointestinal infections. However, they are linked to a number of other side effects, including peripheral neuropathy. They have also been linked to an increased risk of tendon rupture and aortic dissection.
Symptoms of peripheral neuropathy may include tingling, numbness, or pain in the extremities. Although this is not a life-threatening condition, the side effect may lead to a lifetime of medication. Patients may also require revision surgeries or ongoing physical therapy.
Patients taking ciprofloxins should discontinue treatment if they develop symptoms of peripheral neuropathy. Some of these symptoms include pain, burning, tingling, and numbness. These symptoms may occur while the patient is taking ciprofloxins or after the medicine is finished.